Charles J. Goodacre, DDS, MSD, FACP
Loma Linda University School of Dentistry, Loma Linda, CA
Abstract
Technological advances have led to the introduction of 3D education programs specifically designed for dentistry, leading to the author’s use of these programs in the education of dental students. Based on this usage, this paper proposes there are 4 key factors that can enhance student education (spatial ability, interactivity, critical thinking, and clinical correlations with integration of multiple dental disciplines). These key factors can be incorporated into student learning through the use of 3D education programs in class. Lessons learned from using these programs include the importance of regular use in class as well as testing students both visually and textually on the content present in such programs. In this way, students will use the program and thereby enhance their 3D visualization skills while learning the required didactic information. Simply providing students with access to such programs without regular use in class and without testing the students on the content leads to these programs’ lack of use. As a result, the students miss an opportunity to enhance their ability to visualize structures three dimensionally and manipulate them in their minds, a process known as spatial ability that is linked to success in the sciences.
Advances in technology have made it possible to develop enhanced methods of educating students. These methods also serve as learning resources for educators and practitioners. It is now possible to use resources that were only dreamed about as little as 10 years ago. Based on my experience in dental education that spans 4 decades, I would like to propose 4 key factors that enhance learning. Since eHuman (https://ehuman.com/) has developed the only comprehensive educational resources that include 3D resources specifically related to dentistry, I will be providing examples of how their programs can be used to incorporate each of the 4 key factors into student learning.
Key factors that can enhance dental education
Spatial ability
Spatial ability is the process of visualizing a structure and manipulating it in our minds so as to mentally see its form from different views.1 Multiple studies have determined that success in the sciences is related to spatial ability.2-6 Additionally, Wai et al7 examined a stratified random sample of U.S. high school students (N = 400,000) who were tracked for 11+ years. Wai et al stated that their results “solidify the generalization that spatial ability plays a critical role in developing expertise in STEM” (science, technology, engineering, and mathematics). They also reviewed more than 50 years of evidence supporting the relationship between spatial ability and STEM. Another study by Kell et al8 examined 563 intellectually talented 13-year-olds and then examined their creative activities after a time period of more than 30 years. The findings of their study revealed that spatial ability has a unique role in developing creativity and innovation.
A 2017 survey9 of tooth morphology teaching methods used in the United Kingdom and Ireland was sent to 21 individuals at 17 institutions, with 16 surveys being returned. The results indicate that learning the 3D aspects of tooth morphology is important. In addition, the survey respondents agreed that tooth morphology is a difficult course for students. The article concluded by stating that new forms of delivery, such as computer-assisted learning tools, should be used to “help sustain learning and previously acquired knowledge.”
Based on these studies, it seems reasonable to conclude that education resources for dentistry should include 3D programs that enhance our ability to visualize both hard and soft tissues along with associated anatomic structures. In addition, these 3D resources should be used in the education of students in the classroom, in small group settings for students, educators, and practitioners, and during personal study. Also, those courses with laboratory components should focus on the development of spatial abilities through activities that require 3D assessment of the procedures being performed.
Nearly 10 years ago the journal Science published a special section titled “Education and Technology,” highlighting the growing interest in this aspect of education by presenting the perspective of multiple authors. For instance, one author10 concluded that schools often communicate with students using older media, such as print, and rely almost exclusively on the print medium to test knowledge. As science and technology have become increasingly visual, the author indicated there might be a mismatch between the structure of the knowledge and that of the media used to test that knowledge. Furthermore, she went on to state that the “developing human mind needs a balanced diet.”10
In the same special section, Mazur11 stated that “the traditional approach to teaching reduces education to a transfer of information,” while education needs to provide much more. Rather than the early, traditional lecture method where he taught by telling, he now teaches by questioning, with classroom time devoted to discussion of answers. This process actively engages student minds and provides frequent feedback. Mazur concluded his paper with the statement that “evidence is mounting that readjusting the focus of education from information transfer to helping students assimilate material is paying off.” It has been determined that learning is substantially increased when the focus is on students and interactive learning.12 Engaging students during class through interaction with their student peers as they discuss potential answers to questions posed by faculty has caused students to perform better on conceptual assessments and to improve their traditional problem-solving skills.13
Since the 2009 Science publication, technology has improved, knowledge regarding its use has increased, and there is now a deeper understanding of the need for efficiency in learning. Recently, the Journal of the California Dental Association published an issue dealing with the education of millennials. In that issue, a millennial14 discussed the rapid expansion of knowledge through research and the impracticality of expanding the length of dental education to continually encompass the growth in knowledge. As a result, she indicated that mentors and educators need to “find the highest yield examples of what should be taught.” Herein lies an opportunity for technology to help.
The above literature documents the importance of spatial ability, and that knowledge led eHuman to develop multiple education programs specific to dentistry. These programs include a 3D Tooth Atlas, 3D Occlusion Atlas, 3D Head and Neck Anatomy, and 3D Removable Partial Dentures. Acquiring the ability to visualize each of these topics in 3D is important to developing a solid foundation in prosthodontics. Personal experience using these programs during student learning sessions has shown them to be beneficial, while providing faculty with the opportunity to create interactivity in class.
The following are examples of how 3D resources can be used to enhance spatial visualization:
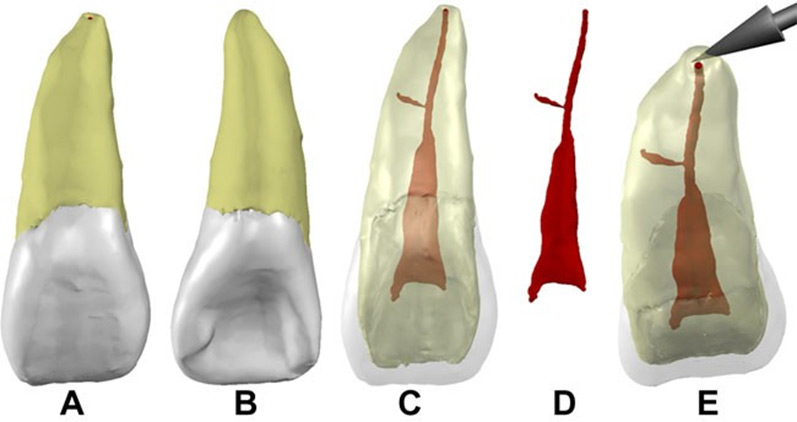
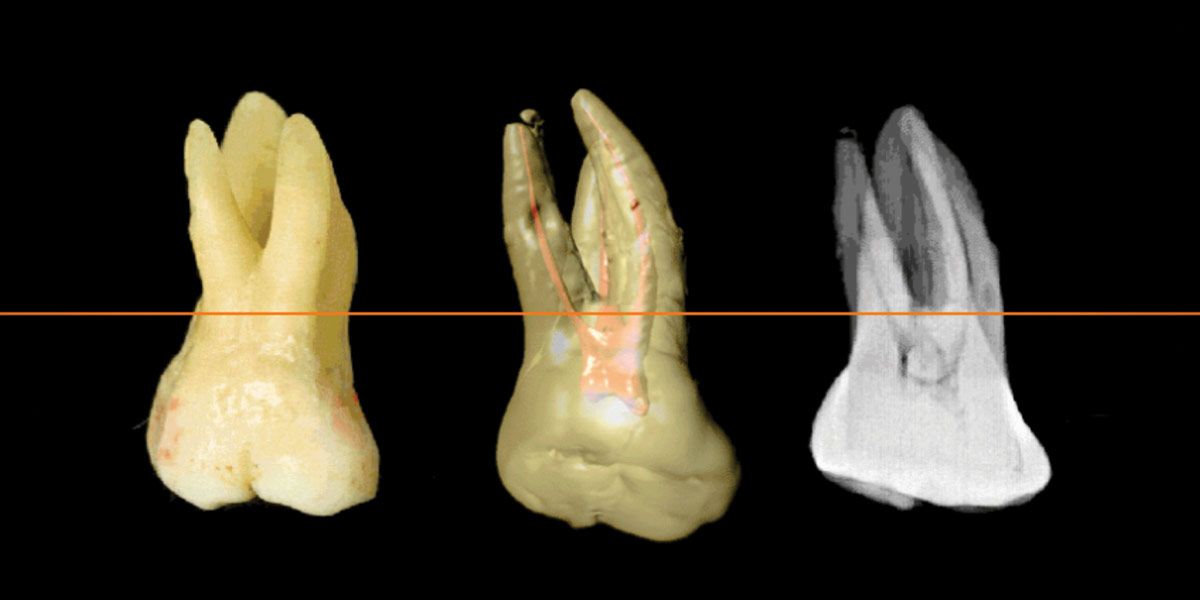
Figure 1. Example of a 3D extracted tooth from eHuman 3D Tooth Atlas. (A) Facial view; (B) tooth rotated to show lingual view; (C) dentin and enamel made partially transparent to show pulp; (D) dentin and enamel made completely transparent to show only the pulp; and (E) tooth angled to show root apex and termination of pulp at the root apex.
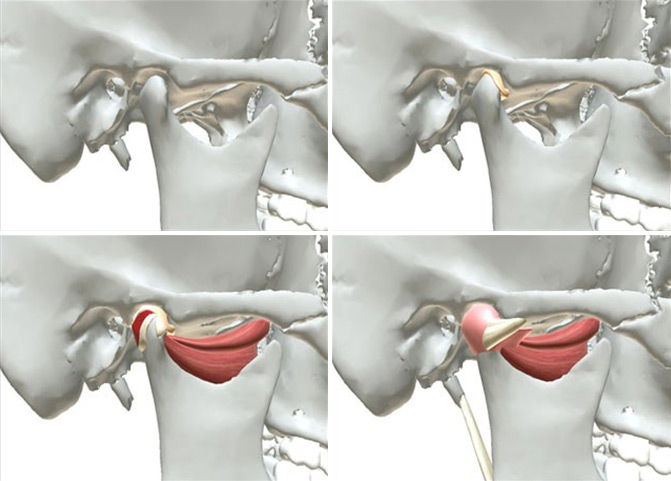
Figure 2. The 3D model of the TMJ. Upper left: the bony components of the joint. Upper right: the articular disc has been added. Lower left: the lateral pterygoid muscle, lateral collateral ligament, and retrodiscal tissue have been added. Lower right: the anterior attachment, capsular ligament, temporomandibular ligament, and stylomandibular ligament have been added.
The 3D Tooth Atlas contains a large virtual library of scanned 3D natural teeth as well as idealized 3D teeth. These virtual teeth can be rotated, zoomed, and moved around the computer screen to view all perspectives of the tooth. The enamel, dentin, and pulp can individually be made opaque, transparent, or be made to disappear (Fig 1). Each tooth can be cross-sectioned. A list of anatomic landmarks provides the ability to label the 3D models. In addition, customized annotations can be added and erased as needed. The teeth can be viewed using augmented reality (AR), where the computer-generated image of the tooth is superimposed on a view of the user’s real world, thus providing a composite view. Also, there is a virtual reality (VR) feature where the teeth can be viewed in realistic 3D using glasses designed for 3D visualization. These features allow students to obtain a true perspective that enhances their ability to see the teeth in their minds and manipulate them. The 3D Occlusion Atlas contains several 3D programs and animations that show mandibular movements and interrelationships of the teeth. It also includes a 3D program that shows how the hard and soft-tissue components of the temporomandibular joint (TMJ) can be individually views or sequentially assembled to create a complete joint while being able to rotate the joint and see it from any view (Fig 2). This program greatly enhances a student’s ability to understand the complexity and function of this unique human joint.
The Removable Partial Denture Program includes 3D models of several types of removable partial denture (RPD) designs. These fully manipulatable 3D models can be effectively used to demonstrate how RPDs function before entering into detailed discussions of individual RPD components or clinical procedures. Each RPD can be placed and removed from its teeth and mucosa to show how it is guided to place, how it fits the teeth, and how it is adapted to the edentulous ridges (Fig 3). The RPD can be individually viewed to show its internal and external surfaces as can the virtual cast with its modified tooth surfaces (Fig 4).
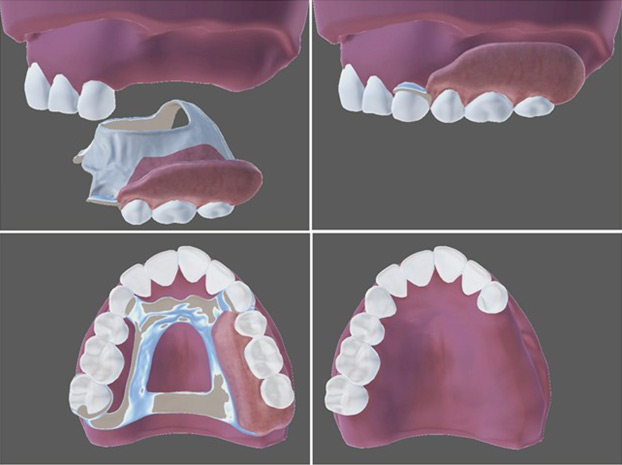
Figure 3. Example of one of the seven different 3D RPD models. Upper left: the RPD is aligned for placement on the virtual cast. Upper right: the RPD has been seated on the cast. Lower left: occlusal view of the RPD seated on the cast. Lower right: the RPD has been turned off to reveal the underlying teeth and residual ridge.
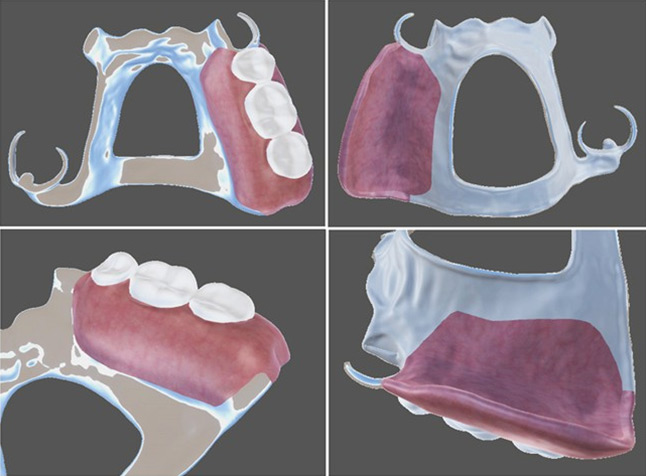
Figure 4. Four views of the RPD with the cast turned off. Upper left: occlusal view showing the polishing framework and resin base. Upper right: intaglio view showing the processed but not polished resin base and the framework finishing that preserves its fit. Lower left: closer view of the external finish line and the metal-to-resin junction with its smooth transition. Lower right: closer view of the internal finish line that has created a smooth metal-to-resin junction.
Interactivity
The previously mentioned special section of the journal Science discussed interactivity and indicated that learning nearly triples with an approach that focuses on the student and on interactive learning. Also, with interactive learning, students performed better on conceptual assessments as well as traditional problem-solving skills. Therefore, methods that can engage students and increase their active participation should be used in both traditional large classroom settings as well as in smaller groups. In fact, one of the reasons small group learning has become more widely used is to enhance student participation with their peers and faculty. As an example of interactivity, I have effectively used the visual self-assessment quizzes in the eHuman 3D Tooth Atlas and the 3D Occlusion Atlas to engage students in class so they actively participate by verbally responding as they recognize different teeth and jaw movements and answer questions based on their visual assessments.
Critical thinking
It is important for all health-care professionals to be able to compare, interpret, summarize, categorize, explain, diagnose, predict, solve, contrast, design, improvise, modify, and innovate. All these words reflect higher levels of learning as opposed to just memorizing facts and are important aspects of the diagnosis and treatment planning of dental patients.
As with interactivity, I have used the self-assessment quizzes in the eHuman 3D Tooth Atlas and the 3D Occlusion Atlas to stimulate critical thinking in class by first having the students answer visual and textual questions and then discussing why the proposed answers were correct or incorrect. Another example is use of the eHuman Removable Partial Denture Program to show students various RPD designs and discuss how the RPD could have been designed differently, along with the reasons some practitioners prefer one design over another.
Clinical correlations with integration of multiple dental disciplines
The completion of a comprehensive dental examination and development of a diagnosis and treatment plan requires the ability to correlate clinical findings with each of the dental disciplines that need to be incorporated into the patient’s treatment plan. Therefore, the presentation of clinical correlations is another key component of a contemporary approach to dental education. Educators15 continue to recognize the need to present topics in the context of patient care and develop curriculum revisions focused on teaching clinically relevant dental anatomy. Because of the importance of relating educational content to patient care, each class period with students should correlate the topic of the period with knowledge from other dental disciplines as well as the basic sciences that can affect patient care. This process should begin with the first classes in dentistry and continue throughout the curriculum so students understand how the information and technical procedures presented in one class relate to other dental sciences and how their integration can enhance the diagnosis and treatment of patients. In this way, students are more likely to have the “big picture” before beginning patient treatment. As an example of how this process can be implemented in class, the 3D virtual teeth in the eHuman 3D Tooth Atlas can be used to show natural morphologic variations as well as abnormalities, areas of incisal/occlusal wear, erosion, caries, and other characteristics that open the door to discussions of their causes, prevention, and management. As another classroom example, use of 3D rotations and slices in the eHuman 3D Tooth Atlas serves as a method of integrating external tooth morphology with computed tomography scan morphology and conventional periapical radiography. Since the 3D Tooth Atlas contains the primary and secondary dentitions as well as pulp morphology, it can be used to help integrate pediatric dentistry, restorative dentistry, endodontics, and radiology.
Discussion
From personal use of eHuman 3D programs and observations at other schools, I have seen that students value these programs, and their learning is enhanced when the programs are used in class by the teacher, and the students are tested both visually and textually on the content contained in the programs.
However, when students acquire a program and it is not used during class and the students are not required to use the resource, it will not be perceived as valuable. After all, students are busy with multiple classes that simultaneously pull their energies in different directions, and they tend not to use peripheral resources when they are not used in class, and quizzes/examinations are not based upon the content in the resource. This observation is no different than requiring students to buy a textbook that is never used in a class. The beneficial use of 3D programs can only be realized when students use the program in class and in their study for quizzes/examinations based on the program content.
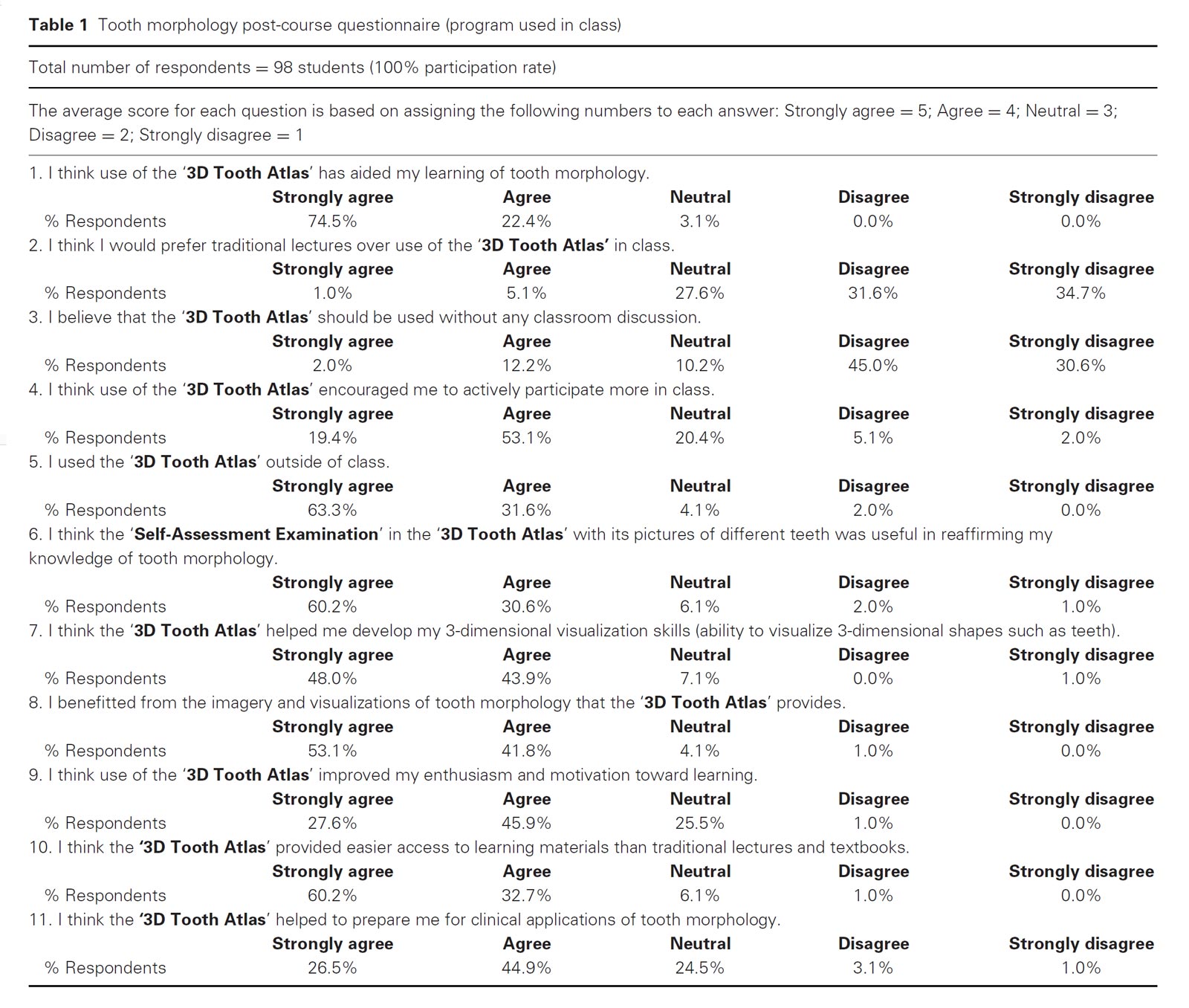
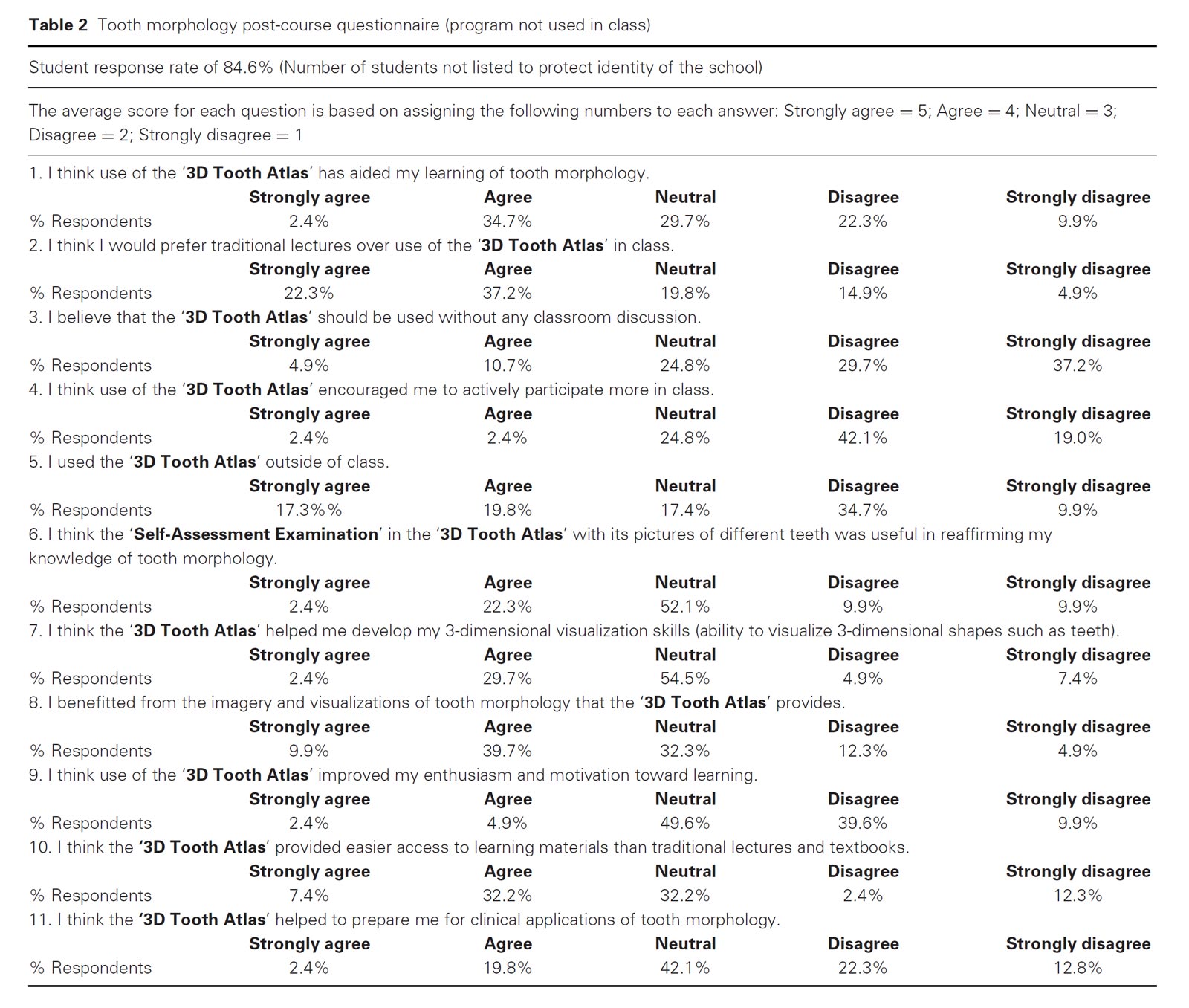
This observation is supported by the results of a survey from a school where the 3D Tooth Atlas was used in class and students were tested on the content in the program, thereby requiring them to use the program (Table 1). The results of that study are in stark contrast to another school where the program was issued to students but was not used in class (Table 2). In fact, a study16 specific to the 3D Tooth Atlas reveals the perspective of students when the program was not regularly used in class and was only provided as an external resource for the class. Students were asked to voluntarily download the program to serve as a study aid. Only 40 of 289 initially downloaded the program, and even after an incentive was added only 126 of 289 students downloaded the program to their laptops.16 As a result, it seems reasonable to conclude that use of such programs by faculty in class along with assignments that require students to use a program is necessary. Otherwise, busy students will not use peripheral aids, and they will not obtain the benefits that could be derived from their usage.
In contrast to the above study, another study17 compared one group of students who did not have access to the 3D Tooth Atlas nor was it used in class, to two other groups that received the software-facilitated learning in each class period and were tested on the content present in the program. The study concluded there was a positive correlation between use of the software program and student performance in final examinations.17 Student perceptions of the program are shown in the post-course survey results presented in Table 1. The results of this survey present a sharp contrast with the survey results presented in Table 2. While neither of these studies definitively proves or disproves the value of using a program such as the 3D Tooth Atlas, they do indicate that classroom use and testing based on the content produces a positive learning experience for students. The focus in learning versus teaching continues to grow, and educators are increasingly recognizing the need to introduce new learner-focused methods into the education of today’s students.18 Rather than continue with traditional lectures presented using PowerPoint or Keynote, it is possible to use software programs as the primary or only source of presenting educational content in unique and engaging ways during both large classroom and small group learning sessions.
In 2018, the eHuman 3D Tooth Atlas became the first comprehensive tooth morphology program to incorporate augmented reality (AR) and virtual reality (VR). These features present an educational opportunity that needs to be explored to determine if such features can enhance a student’s ability to visualize teeth 3-dimensionally as well as explore student perceptions of benefits and limitations. A recent study19 determined the use of 3D software had a positive effect on student performance; however, publications related to AR/VR in dentistry are very limited,20,21 and they are not specifically related to student education.
In a nursing study22 students demonstrated their ability to place a nasogastric tube by either watching an animated video and reading information or using an iPad AR virtual simulation training module. The AR module was perceived more positively by the students regarding realism, ease of use, and the ability to identify landmarks and visualize internal organs. Also, it promoted student learning and understanding.22 However, studies in the health sciences are very limited. In fact, a systematic review by Bacca et al23 reported that health education is one of the fields where AR has been least explored. In contrast, there have been a number of studies and systematic reviews in other fields.
A review of AR by Radu24 presented a list of learning benefits that included increased content understanding, long-term memory retention, improved physical task performance, improved student collaboration, and increased student motivation. Similarly, in the above cited review by Bacca et al23 the main advantages of AR were listed as gains in learning, motivation, interaction, and collaboration. Negative aspects of AR24 include attention tunneling (high attention demands causing students to miss important aspects of the experience or feeling unable to perform team tasks), difficulty in using AR systems, decreased student engagement in class, and variation in the learning benefits with different students.
A Cochrane Database Systematic Review25 of VR training for ear, nose, and throat surgery included 9 studies. The authors concluded there is limited evidence to support VR simulation in surgical training programs, and further investigations are needed to determine if better technical skills are developed and if better outcomes are obtained for patients. Another Cochrane Database Systematic Review26 of VR training in laparoscopic surgery concluded that such training appears to decrease the operating time and improve the surgical performance of trainees with limited laparoscopic experience. A third Cochrane review27 of VR training for gastrointestinal endoscopy concluded that endoscopy training can be an effective supplement, but there is insufficient evidence to support its use as a replacement for the conventional apprenticeship model of training. Another systematic review28 of VR training for laparoscopic surgery determined that VR training was more accurate than video training and resulted in decreased operating time and fewer errors and unnecessary movements.
Conclusions
Based on the reviewed studies and the observations of the author, the following conclusions are offered:
- Spatial ability (the ability to visualize a structure and manipulate it in the mind so as to mentally see its form from different perspectives) contributes to success in the
- Dental education should include 3D resources that enhance the ability of students to visualize both hard and soft
- There are 3D education programs that can be used in class to enhance spatial
- Interactivity in class can enhance student
- It is important to include critical thinking in the education of
- Dental courses should include clinical correlations with the other disciplines of dentistry and the basic
- The effective use of 3D education programs requires that they be regularly used in class and that students are tested on the content present in the
- The introduction of AR and VR into dentistry offers an opportunity to study the perceptions of students regarding their benefits and limitations as well as to determine if they enhance a student’s 3D visualization skills.
References
- Hegarty M, Waller DA: Individual differences in spatial In Shah P, Miyake A (eds): The Cambridge Handbook of Visuospatial Thinking. Cambridge, Cambridge University Press, 2005
- Garg AX, Norman G, Sperotable L: How medical students learn spatial anatomy. Lancet 2001;357:363-364
- Hegarty M, Keehner M, Khooshabeh P, et al: How spatial abilities enhance, and are enhanced by, dental education. Learn Individ Differences 2009;19:61-70
- Harle M, Towns M: A review of spatial ability literature, its connection to chemistry, and implications for J Chem Educ 2011;88:351-360
- Orien N, Ben-Chaim D, Kall Y: Relationship between earth-science education and spatial visualization. J Geosci Educ 1997;45:129-132
- Kozhevnikov M, Motes MA, Hegarty M: Spatial visualization in physics problem solving. Cogn Sci 2007;31:549-579
- Wai J, Lubinski D, Benbow CP: Spatial ability from STEM domains: Aligning over 50 years of cumulative psychological knowledge solidifies its importance. J Educ Psych 2009;101:817-835
- Kell HJ, Lubinski D, Benbow CP, et al: Creativity and technical innovation: Spatial’s ability’s unique role. Psych Sci 2013;24:1831-1836
- Lone M, McKenna P, Cryan F, et al: A survey of tooth morphology teaching methods employed in the United Kingdom and Ireland. Eur J Dent Educ 2018;22:e438-e443
- Greenfield PM: Technology and information education: What is taught, what is learned. Science 2009;323:69-71
- Mazur E: Farewell, lecture? Science 2009;323:50-51
- Fagen AP, Crouch CH, Mazur E: Peer instruction: results from a range of classrooms. Phys Teach 2002;40:206-209
- Crouch CH, Mazur E: Peer instruction: ten years of experience and results. Am J Phys 2001;69:970-977
- Greene CC: How to educate millennials. J Calif Dent Assoc 2018;46:359-362
- Obrez A, Briggs C, Buckman J, et al: Teaching clinically relevant dental anatomy in the dental curriculum: description and assessment of an innovative module. J Dent Educ
2011;75:797-804 - Wright EF, Hendricson WD: Evaluation of a 3-D interactive tooth atlas by dental students in dental anatomy and endodontics courses. J Dent Educ 2010;74:110-122
- Al-Thobity AM, Farooq I, Khan SQ: Effect of software facilitated teaching on final grades of dental students in a dental morphology course. Saud Med J 2017;38:192-195
- Donnelly R, Fitzmaurice M: Collaborative project-based learning and problem-based learning in higher education. A consideration of tutor and student role in learner-focused strategies. In O’Neill G, Moore S, McMullin B (eds): Emerging Issues in the Practice of University Learning and Dublin, AISHE/HEA, 2005, pp 87–95
- Hu J, Yu H, Shao J, et al: Effects of dental 3D multimedia system on the performance of junior dental students in preclinical practice: a report from China. Adv Health Sci Educ Theory Pract 2009;14:123-133
- Huang TK, Yang CH, Hsieh YH, et al: Augmented reality (AR) and virtual reality (VR) applied to dentistry. Kaohsiung J Med Sci 2018;34:243-248
- Albuha Al-Mussawi RM, Farid F: Computer-based technologies in dentistry: types and applications. J Dent (Tehran) 2016;13:215-222
- Aerbersold M, Voepel-Lewis T, Cherara L, et al: Interactive anatomy-augmented virtual simulation training. Clin Simul Nurs 2018;15:34-41
- Bacca J, Baldiris S, Fabregat R, et al: Augmented reality trends in education: a systematic review of research and application. Educ Tech Soc 2014;17:133-149
- Radu I: Augmented reality in education: a meta-review and cross-media analysis. Pers Ubiquit Comput 2014;18:
1533-1543 - Piromchai P, Avery A, Laopaiboon M, et al: Virtual reality training for improving the skills needed for performing surgery of the ear, nose, and throat. Cochrane Database Syst Rev 2015 Sep 9;(9):CD010198. https://doi.org/10.1002/14651858.CD010198. pub2
- Nagendran M, Gurusamy KS, Aggarwal R, et al: Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 2014 Mar 1;(3):CD010478. https://doi.org/10.1002/14651858.CD010478.pub2. Review
- Walsh CM, Sherlock ME, Ling SC, et al: Virtual reality simulation training for health professions trainees in gastrointestinal Cochrane Database Syst Rev 2012 Jun 13;(6):CD008237. https://doi.org/10.1002/14651858.CD008237.pub2. Review
- Gurusamy K, Aggarwal R, Palanivelu L, et al: Systematic review of randomized controlled trials on the effectiveness of virtual reality training for laparoscopic surgery. Br J Surg
2008;95:1088-1097